 | Element 1: An institution-specific antimicrobial stewardship policy and/or procedure has been adopted.
A formal ASP policy defines the goals and scope of the ASP, and takes into consideration the needs of the healthcare facility. There is no single template for an ASP; the following documents illustrate examples of how to frame the purpose and rationale of an ASP and define the scope of ASP activities. |
 | Element 2: A physician-supervised multidisciplinary antimicrobial stewardship committee or workgroup has been convened.
The ASP committee oversees organization-wide efforts to promote and evaluate the appropriate use of antimicrobial agents. Ideally, the committee membership should include physician stakeholders who act as liaisons/champions to promote stewardship education and practices among their various services and disciplines. |

| Element 3: ASP leadership support is provided by a physician or pharmacist with antimicrobial stewardship training from a recognized professional organization or post-graduate education.
Formal training in antimicrobial stewardship benefits ASP leaders, who must possess medical infection disease and microbiology knowledge and understand how to start and maintain an ASP, including how to implement change and measure success of a program. Training requirements may be met through several continuing education training programs offered by the federal Centers for Disease Control and Prevention, the Society for Healthcare Epidemiology of America, and/or other recognized professional organizations.
Examples of antimicrobial stewardship education and training courses: |
 | Element 4: ASP activities are routinely reported to hospital quality improvement committees.
Dissemination of information about ASP activities is an important means of promoting stewardship across the hospital, and emphasizes to key stakeholders the role and value of ASPs in promoting quality and safe patient care. Engaging hospital committees involved in quality improvement (QI) helps promote ongoing evaluation and improvement of the program. Discussing challenges with experts can foster creative solutions. The following examples demonstrate ASP reports to hospital QI committees. |
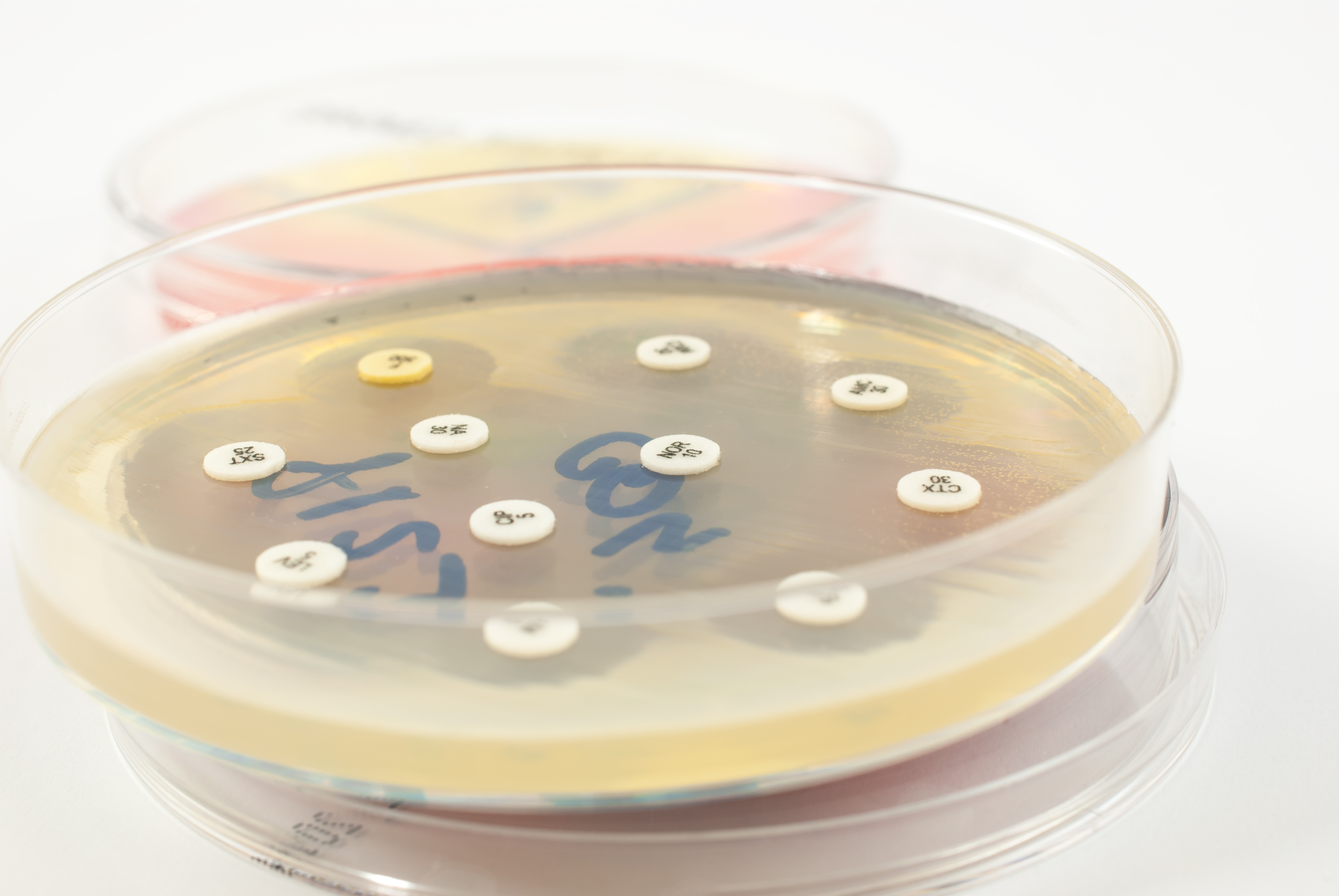 | Element 5: An annual antibiogram is developed using Clinical laboratory Standards Institute guidelines and distributed to medical staff, with follow-up education provided.
An antibiogram is a summary report of antimicrobial susceptibilities of selected pathogens using Clinical Laboratory Standards Institute (CLSI) criteria. Antibiograms reflect the percentage of a given organism that is susceptible to each of the antimicrobial agents routinely tested. Local antibiograms with pathogen-specific susceptibility data should be updated annually to provide guidance to clinicians on choosing appropriate empiric therapy. |

| Element 6: Institutional guidelines have been developed for the management of common infection syndromes (e.g. order sets, clinical pathways, empiric antimicrobial therapy guides).
Development of evidence-based clinical management guidelines that incorporate local microbiology and resistance patterns can improve antimicrobial utilization. Guideline adherence can be facilitated through provider education, use of electronic order sets, guideline distribution on websites or mobile applications, and provider feedback on antimicrobial use and patient outcomes. Examples of institutional guidelines: |
 | Element 7: Usage patterns of antibiotics determined to be of importance to the resistance ecology of the facility are monitored using defined daily dosing (DDD) or days of therapy (DOT).
Measurement of aggregate usage of antimicrobials in a healthcare facility can help to optimize antimicrobial utilization and patient outcomes. Techniques for aggregate measurement of antimicrobial use will vary based on the available data and resources at each institution. DDD or DOT are the preferred units of measurement. Example 7.1: Measuring Antimicrobial Use: A Step-by-Step Guide, University of California San Francisco Medical Center |

| Element 8: Regular antimicrobial stewardship education provided to medical staff and committees.
One of the most important aspects of an effective ASP is the dissemination of stewardship education and metrics data to medical staff. Practitioners are much more likely to change their prescribing habits when local data are presented that demonstrate opportunities for improvement. Education can be provided in any number of ways, including regular reports at medical staff or departmental meetings, monthly newsletters, and regular conferences or grand rounds. Example 8.1: Newsletter, Children’s Hospital and Research Center
Example 8.2: Medical Director’s Report, Sutter Eden Medical Center
Example 8.3: Newsletter, Palomar Health Newsletter |
 | Element 9: The antimicrobial formulary is reviewed annually and changes made based on local antibiogram.
The local annual antibiogram provides essential information to guide empiric antimicrobial therapy pending final culture results. The microbiology laboratory should provide an antibiogram for analysis on an annual basis at a minimum. The ASP committee should review, make changes to the formulary and order sets to ensure that the options are congruent with the antimicrobial susceptibility patters seen on the most recent antibiogram. Periodic education of providers should be based on this analysis and any resulting changes to the formulary and order sets. |
 | Element 10: Prospective audits of antimicrobial prescriptions are performed and intervention/feedback is provided to prescribers.
Prospective audits with intervention and feedback to the prescriber have been demonstrated to improve appropriate antimicrobial use. This process allows the ASP to identify opportunities for optimization of antimicrobial therapy by addressing antimicrobial choice, dosing, route, and/or duration. The feedback process serves as an opportunity for one-on-one education of prescribers. |