What general strategies can be used to reduce environmental bioburden?Improve the cleaning and disinfection of rooms after discharge of patients/residents known to carry healthcare-associated pathogens, such as CDI Daily clean and disinfect all high-touch surfaces Clean and disinfect portable equipment Improve cleaning and disinfection of all rooms and areas of the healthcare facility
Donskey. AJIC. 2013 (read article via PubMed) |
What is cleaning? Why must an object or surface be cleaned prior to being disinfected?Cleaning removes large numbers of microorganisms from a surface that would otherwise interfere with the disinfection process Disinfectants are not as effective in the presence of organic material Important: A thorough cleaning must occur before a surface can be disinfected
HICPAC /CDC 2003 (read Guidelines for Environmental Infection Control via CDC)
HICPAC /CDC 2008 (read Guideline for Disinfection and Sterilization via CDC) |
What is the difference between a detergent and a disinfectant?- Detergent
- A cleaning agent that contains surfactants; lifts dirt
- Does not kill microorganisms
- Can become easily contaminated
- Less toxic, less odor and less costly than disinfectant
- Disinfectant
- Inhibits growth and/or kills microorganisms
- Also referred to as a germicide, which is a disinfectant that kills organisms that can cause disease
- More toxic, more odor, and more costly than detergent
Pyrek K, Emerging Pathogens and Environmental Cleaning, ICT, 2015 (read report via Infection Control Today) Chou. APIC Text of Infection Control & Epidemiology. 2013 (read atricle via APIC Text Online) |
What are the factors that influence selection of disinfectant?- Nature of the item to be disinfected
- Amount of organic soil present
- Number of microorganisms present
- Innate resistance of microorganisms to the inactivating effects of the germicide
- Type and concentration of germicide used
- Duration and temperature of germicide contact
- Other specific indications and directions for use
HICPAC /CDC 2003 (read Guidance via CDC) |
What are the different antisepsis, disinfection, and sterilization types, actions, and resistance? Not all microorganisms are the same. Some are more resistant to disinfection than others and require stronger germicides to eliminate. Viruses, fungi, and bacteria, including MRSA, VRE and CRE, can be eliminated with germicides containing quaternary ammonium compounds (“Quat”) or organic acids. Mycobacteria, including TB (and viruses, fungi, and bacteria as above) can be eliminated with germicides containing a phenols, Quat plus alcohol, iodophors or alcohols. Bacterial spores, including C. difficile (and viruses, fungi, and bacteria, and mycobacteria as above) require germicides containing hypochlorites (bleach at the recommended dilution), aldehydes, peroxides, chlorine dioxide, or ethylene oxide
Bacterial spores including Clostridium difficile are in the most resistant category of microorganisms. 
Adapted from: McDonnell G. Antisepsis, disinfection and sterilization: types, action and resistance. 2007. Used with permission from EcoLab © 2011 |
What is an EPA label claim? What should I look for on an EPA label?Chemical germicides are regulated by the Environmental Protection Agency (EPA) The EPA label claim states if the product is bactericidal, virucidal, tuberculocidal, fungicidal, or sporicidal The label clarifies the manufacturer's instructions for use, including wet contact time required to achieve the desired degree of microbial killing
CDC. MMWR. Dec 19, 2003 (read Guidelines for Environmental Infection Control via CDC) Pyrek K, Emerging Pathogens and Environmental Cleaning, ICT, 2015 (read report via Infection Control Today) Rutala et al. ICHE. 2014 (read article via PubMed) |
Why is bleach or a disinfectant with a sporicidal claim used to clean CDI patient rooms?Strategies to Prevent C. difficile in Acute Care Facilities (read strategies via CDC)
LIST K: EPA’s Registered Antimicrobial Products Effective against Clostridium difficile Spores (read list via EPA) |
What is wet contact time? Why is it important and required?The time required for a disinfectant to kill microorganisms on a pre-cleaned surface The disinfectant must remain wet long enough to achieve the claimed level of surface disinfection Follow manufacturer's guidelines for achieving the appropriate wet contact time
Rutala et al. ICHE. 2014 (read article via PubMed) |
What are best practices for efficiently cleaning a patient care room? Ensure proper hand hygiene and use of gloves Focus on frequently touched surfaces Work from clean-to-dirty and high-to-low areas Avoid generating aerosols Change cleaning cloths after cleaning a heavily soiled area or surface (i.e. toilet) and when going from one area to another Ensure equipment and supplies are clean Ensure proper use of cleaning and disinfecting products Remember: A surface must be physically cleaned before it can be disinfected Communicate issues to your supervisors
Public Health Ontario, Environmental Cleaning Top 10 Best Practices (read presentation via HealthUnit.org) |
Is there evidence that the environmental cleaning with bleach can reduce CDI rates on high-incidence units?Bleach solution has been shown to be effective in decreasing patients' risk of developing CDI on high-incidence units. In one study, a significant reduction in CDI incidence was observed when bleach solution was used as an environmental disinfectant ("intervention" period) on the unit with highest baseline CDI incidence The CDI rate reversed to the baseline CDI rate when a quaternary ammonium was used ("post-intervention" period). No reductions in CDIs were observed when bleach solution was used as environmental disinfectant on the units with lower baseline CDI rates.
Mayfield et al. Clin Infect Dis. 2000 (read article via PubMed) |
Where can I find additional resources with best practices for efficiently cleaning a room?A CDC Toolkit contains example list of frequently touched surfaces and checklists for monitoring cleaning The Minnesota Hospital Association published a Controlling CDI: Environmental Services Cleaning Guidebook
Environmental Services Cleaning Guide: Controlling CDI (read Guidebook via Minnesota Hospital Association) Hota. CID. 2004 (read article via PubMed) |
What are cleaning considerations if a CDI patient shares a room with a non-CDI patient?Place CDI patient furthest from the door to minimize dirty-to-clean area traffic Focus on high-touch surfaces and equipment in the immediate vicinity of patient/resident separately Mop on non-CDI patient's side first; mops should only be used in the one room Change cleaning cloths after use on one side of the room only Change privacy curtains more frequently
2007 HICPAC Isolation Guidelines (read Isolation Guidleines via CDC) |
What are ways to ensure EVS staff adhere to hand hygiene practices?Emphasize the importance of hand hygiene for EVS staff in helping to prevent infections Change misconception that hand hygiene is only important for protecting EVS staff. Emphasis that EVS hand hygiene is for protecting patients Orient EVS staff thoroughly to infection control principles and practices prior to starting work in a clinical area
Lillis K, Hand Hygiene: EVS Personnel Play Key Role in Preventing Spread of Infection, ICT, 2015 (read article via Infection Control Today) |
What personal protective equipment (PPE) should be used while cleaning?Choice of PPE is based on: Refer to the Material Safety Data Sheet (MSDS), directions sheet, and facility policy Appropriate use of PPE is critical
Tomas et al. JAMA Int Med. 2015 (read article via PubMed) |
Which is better for cleaning cloths: microfiber or cotton?Microfiber Densely constructed synthetic strands Attracts dust, cleans 50% better than comparable cotton Easier to use, lighter, designed for repeat usage In a UC Davis study, microfiber was initially more expensive than cotton, but cleaned better, used less water and chemicals, and decreased labor costs.
UC Davis Case Study. Nov 2002 (read article via US Environmental Protection Agency) Trajtman. AJIC. 2015 (read article via PubMed) Smith. J Hosp Infect. 2011 (read article via PubMed) HICPAC / CDC 2008 (read Guideline for Disinfection and Sterilization via CDC) Microfiber (top) Cotton (bottom) 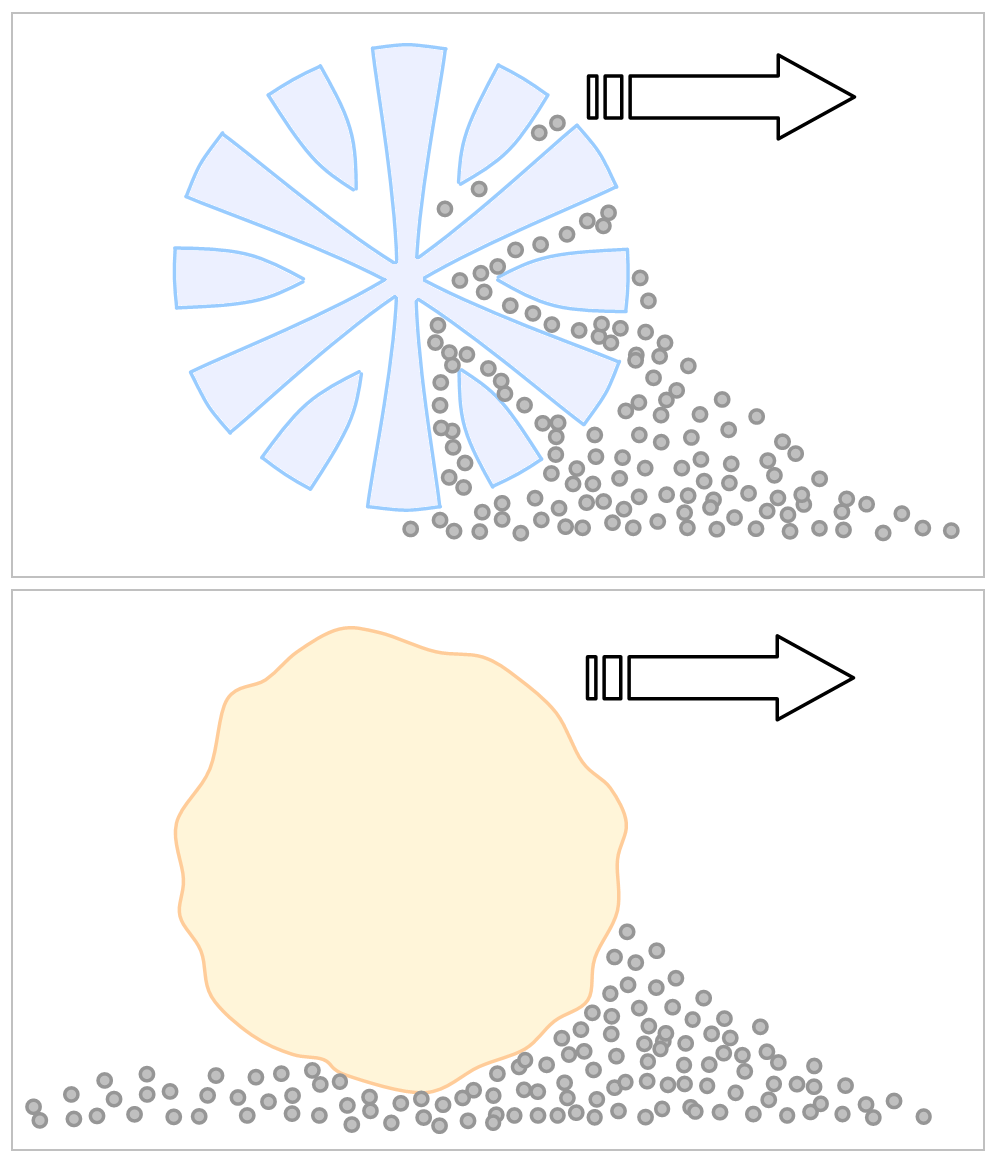
|
What is the best way to clean porous surfaces such as a fabric chair or carpeting?Fabric should be regularly vacuumed and re-covered when worn Organic material and excess liquid should be extracted as much as possible Steam cleaning is recommended for carpets as appropriate; carpets should be allowed to dry for 72 hours to prevent growth of fungi No epidemiological evidence to show that pathogens found on fabric are linked to increased risk of HAIs
MMWR. 2003 (read Guidelines for Environmental Infection Control via CDC) Chou. APIC Text of Infection Control & Epidemiology. 2013 (read article via APIC Text Online) |
Summary of Key PointsA properly cleaned care environment is essential to prevent or contain HAIs A surface must be physically cleaned before it can be disinfected Consistent use of best practices and clarity of roles should be emphasized Use of technologies such as microfiber, monitoring systems, and whole-room disinfection after cleaning are increasingly becoming the community standard of care EVS staff should be valued and supported so they can maximize their unique contributions to preventing HAI
|